References:
1. Foreman, P. K. et al. Birth prevalence of achondroplasia: a systematic literature review and meta-analysis. Am. J. Med. Genet. A 182, 2297–2316 (2020).
2. Horton, W. A., Hall, J. G. & Hecht, J. T. Achondroplasia. Lancet 370, 162–172 (2007).
3. Pauli, R. M. Achondroplasia: a comprehensive clinical review. Orphanet J. Rare Dis. 14, 1 (2019).
4. Savarirayan, R. & Rimoin, D. L. Skeletal dysplasias. Adv. Pediatr. 51, 209–229 (2004).
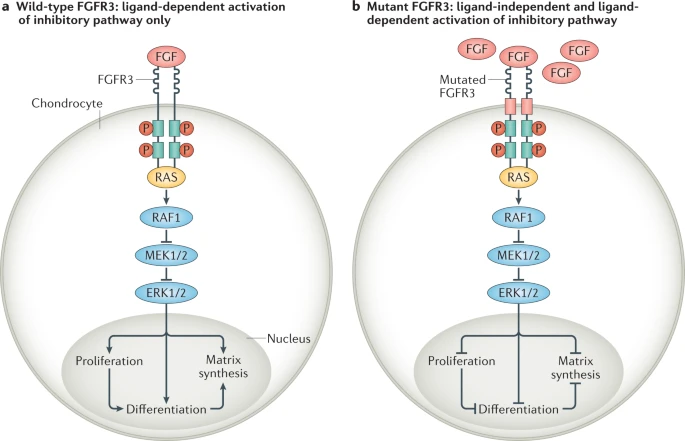
5. Legeai-Mallet, L. & Savarirayan, R. Novel therapeutic approaches for the treatment of achondroplasia. Bone 141, 115579 (2020).
6. Savarirayan et al. Best practice guidelines regarding prenatal evaluation and delivery of patients with skeletal dysplasia. Am. J. Obstet. Gynecol. 219, 545–562 (2018).
7. Giles, C. Multidisciplinary team meetings having both patient advocates and patients at the MDT meeting might be useful. BMJ 351, 0008 (2015).
8. Wright, M. J. & Irving, M. D. Clinical management of achondroplasia. Arch. Dis. Child. 97, 129–134 (2012).
9. Dwek, J. R. A framework for the radiologic diagnosis of skeletal dysplasias and syndromes as revealed by molecular genetics. Pediatr. Radiol. 49, 1576–1586 (2019).
10. Offiah, A. C. & Hall, C. M. The radiologic diagnosis of skeletal dysplasias: past, present and future. Pediatr. Radiol. 50, 1650–1657 (2020).
11. Watson, S., Calder, A., Offiah, A. & Negus, S. A review of imaging protocols for suspected skeletal dysplasia and a proposal for standardisation. Pediatr. Radiol. 45, 1733–1737 (2015).
12. White, K. K. et al. Best practices in peri-operative management of patients with skeletal dysplasias. Am. J. Med. Genet. A 173, 2584–2595 (2017).
13. Ireland, P. J. et al. Development in children with achondroplasia: a prospective clinical cohort study. Dev. Med. Child Neurol. 54, 532–537 (2012).
14. Trotter, T. L. & Hall, J. G. Health supervision for children with achondroplasia. Pediatrics 116, 771–783 (2005).
15. Ireland, P. J. et al. Optimal management of complications associated with achondroplasia. Appl. Clin. Genet. 7, 117–125 (2014).
16. Cheung, M. S. et al. Achondroplasia foramen magnum score: screening infants for stenosis. Arch. Dis. Child. 106, 180–184 (2021).
17. Nadel, J. L., Wilkinson, D. A., Garton, H. J. L., Muraszko, K. M. & Maher, C. O. Screening and surgery for foramen magnum stenosis in children with achondroplasia: a large, national database. Anal. J. Neurosurg. Pediatr. 23, 374–380 (2019).
18. Tunkel, D. E. et al. Hearing screening in children with skeletal dysplasia. Arch. Otolaryngol. Head Neck Surg. 137, 1236–1239 (2011).
19. Alade, Y. et al. Cross-sectional assessment of pain and physical function in skeletal dysplasia patients. Clin. Genet. 84, 237–243 (2013).
20. Fredwall, S. O. et al. High prevalence of symptomatic spinal stenosis in Norwegian adults with achondroplasia: a population-based study. Orphanet J. Rare Dis. 15, 123 (2020).
21. Lee, S. T. et al. Development of genu varum in achondroplasia. J. Bone Joint Surg. Br. 89-B, 57–61 (2007).
22. Dhiman, N. et al. Factors associated with health-related quality of life (HRQoL) in adults with short stature skeletal dysplasias. Qual. Life Res. 26, 1337–1348 (2017).
23. Jennings, S. et al. Prevalence of mental health conditions and pain in adults with skeletal dysplasia. Qual. Life Res. 28, 1457–1464 (2019).
24. Wynn, J., King, T. M., Gambello, M. J., Waller, D. K. & Hecht, J. T. Mortality in achondroplasia study: a 42-year follow-up. Am. J. Med. Genet. A 143A, 2502–2511 (2007).
25. Yonko, E. A., Emanuel, J. S., Carter, E. M. & Raggio, C. L. Quality of life in adults with achondroplasia in the United States. Am. J. Med. Genet. A 185, 695–701 (2021).
26. Shakespeare, T., Thompson, S. & Wright, M. No laughing matter: medical and social experiences of restricted growth. Scand. J. Disabil. Res. 12, 19–31 (2010).
27. Hoover-Fong, J., Scott, C. I. & Jones, M. C. Health supervision for people with achondroplasia. Pediatrics 145, e20201010 (2020).
28. Del Pino, M., Fano, V. & Lejarraga, H. Growth references for height, weight, and head circumference for Argentine children with achondroplasia. Eur. J. Pediatr. 170, 453–459 (2011).
29. Hoover-Fong, J., McGready, J., Schulze, K., Alade, A. Y. & Scott, C. I. A height-for-age growth reference for children with achondroplasia: expanded applications and comparison with original reference data. Am. J. Med. Genet. A 173, 1226–1230 (2017).
30. Merker, A. et al. Development of body proportions in achondroplasia: sitting height, leg length, arm span, and foot length. Am. J. Med. Genet. A 176, 1819–1829 (2018).
31. Neumeyer, L., Merker, A. & Hagenäs, L. Clinical charts for surveillance of growth and body proportion development in achondroplasia and examples of their use. Am. J. Med. Genet. A 185, 401–412 (2021).
32. Tofts, L., Das, S., Collins, F. & Burton, K. L. O. Growth charts for Australian children with achondroplasia. Am. J. Med. Genet. A 173, 2189–2200 (2017).
33. Ireland, P. J. et al. Functional performance in young Australian children with achondroplasia. Dev. Med. Child Neurol. 53, 944–950 (2011).
34. Pauli, R., Breed, A., Horton, V., Glinski, L. & Reiser, C. Prevention of fixed, angular kyphosis in achondroplasia. J. Pediatr. Orthop. 17, 726–733 (1997).
35. Sanders, V. R., Sheldon, S. H. & Charrow, J. Cervical spinal cord compression in infants with achondroplasia: should neuroimaging be routine? Genet. Med. 21, 459–463 (2019).
36. Savarirayan, R. et al. Best practice guidelines in managing the craniofacial aspects of skeletal dysplasia. Orphanet J. Rare Dis. 16, 31 (2021).
37. Esposito, S. & Principi, N. Immunization against pertussis in adolescents and adults. Clin. Microbiol. Infect. 22, S89–S95 (2016).
38. Hashmi, S. S. et al. Multicenter study of mortality in achondroplasia. Am. J. Med. Genet. A 176, 2359–2364 (2018).
39. Simmons, K., Hashmi, S. S., Scheuerle, A., Canfield, M. & Hecht, J. T. Mortality in babies with achondroplasia: revisited. Birth Defects Res. A Clin. Mol. Teratol. 4, 247–249 (2014).
40. Bosemani, T. et al. Achondroplasia in children: correlation of ventriculomegaly, size of foramen magnum and jugular foramina, and emissary vein enlargement. Childs Nerv. Syst. 31, 129–133 (2015).
41. Moritani, T. et al. Magnetic resonance venography of achondroplasia: correlation of venous narrowing at the jugular foramen with hydrocephalus. Clin. Imaging 30, 195–200 (2006).
42. White, K. K. et al. Best practices in the evaluation and treatment of foramen magnum stenosis in achondroplasia during infancy. Am. J. Med. Genet. A 170, 42–51 (2016).
43. Cheung, M. S., Alves, I., Hagenäs, L. & Mohnike, K. Meeting report from the achondroplasia foramen magnum workshop, Salzburg, Austria 22nd June 2019. Bone 127, 499–502 (2019).
44. Hoover-Fong, J. et al. Achondroplasia Natural History Study (CLARITY): a multicenter retrospective cohort study of achondroplasia in the United States. Genet. Med. 23, 1498–1505 (2021).
45. King, J. A. J., Vachhrajani, S., Drake, J. M. & Rutka, J. T. Neurosurgical implications of achondroplasia: a review. J. Neurosurg. Pediatr. 4, 297–306 (2009).
46. Calandrelli, R. et al. Quantitative approach to the posterior cranial fossa and craniocervical junction in asymptomatic children with achondroplasia. Neuroradiology 59, 1031–1041 (2017).
47. Rekate, H. L. The unique challenge of hydrocephalus in achondroplasia. Fluids Barriers CNS 16, O67 (2019).
48. Mackenzie, W. G. et al. Flexion-extension cervical spine MRI in children with skeletal dysplasia: is it safe and effective? J. Pediatr. Orthop. 33, 91–98 (2013).
49. Brouwer, P., Lubout, C., Dijk, J. & Vleggeert-Lankamp, C. Cervical high-intensity intramedullary lesions in achondroplasia: aetiology, prevalence and clinical relevance. Eur. Radiol. 22, 2264–2272 (2012).
50. Davies, J. M., Ozpinar, A. & Lawton, M. T. Volume-outcome relationships in neurosurgery. Neurosurg. Clin. N. Am. 26, 207–218 (2015).
51. Fornarino, S. et al. Early impairment of somatosensory evoked potentials in very young children with achondroplasia with foramen magnum stenosis. Dev. Med. Child Neurol. 59, 192–198 (2017).
52. Van Dijk, J. M. C., Lubout, C. M. A. & Brouwer, P. A. Cervical high-intensity intramedullary lesions without spinal cord compression in achondroplasia. J. Neurosurg. Spine 6, 304–308 (2007).
53. Del Pino, M., Ramos Mejía, R. & Fano, V. Leg length, sitting height, and body proportions references for achondroplasia: new tools for monitoring growth. Am. J. Med. Genet. A 176, 896–906 (2018).
54. Miccoli, M., Bertelloni, S. & Massart, F. Height outcome of recombinant human growth hormone treatment in achondroplasia children: a meta-analysis. Horm. Res. Paediatr. 86, 27–34 (2016).
55. Hertel, N. T. et al. Growth hormone treatment in 35 prepubertal children with achondroplasia: a five-year dose-response trial. Acta Paediatr. 94, 1402–1410 (2005).
56. Ireland, P. J. et al. Medical management of children with achondroplasia: evaluation of an Australasian cohort aged 0–5 years. J. Paediatr. Child Health 48, 443–449 (2012).
57. Misra, S. N. & Morgan, H. W. Thoracolumbar spinal deformity in achondroplasia. Neurosurg. Focus. 14, e4 (2003).
58. Hoover-Fong, J. E., McGready, J., Schulze, K. J., Barnes, H. & Scott, C. I. Weight for age charts for children with achondroplasia. Am. J. Med. Genet. A 143A, 2227–2235 (2007).
59. Hoover-Fong, J. E., Schulze, K. J., McGready, J., Barnes, H. & Scott, C. I. Age-appropriate body mass index in children with achondroplasia: interpretation in relation to indexes of height. Am. J. Clin. Nutr. 88, 364–371 (2008).
60. Saint-Laurent, C., Garde-Etayo, L. & Gouze, E. Obesity in achondroplasia patients: from evidence to medical monitoring. Orphanet J. Rare Dis. 14, 253 (2019).
61. Sims, D., Onambélé-Pearson, G., Burden, A., Payton, C. & Morse, C. Whole-body and segmental analysis of body composition in adult males with achondroplasia using dual X-ray absorptiometry. PLoS One 14, e0213806 (2019).
62. De Vries, O. M., Johansen, H. & Fredwall, S. O. Physical fitness and activity level in Norwegian adults with achondroplasia. Am. J. Med. Genet. A 185, 1023–1032 (2021).
63. Ain, M. C., Shirley, E. D., Pirouzmanesh, A., Hariri, A. & Carson, B. S. Postlaminectomy kyphosis in the skeletally immature achondroplast. Spine 31, 197–201 (2006).
64. Borkhuu, B., Nagaraju, D. K., Chan, G., Holmes, L. & Mackenzie, W. G. Factors related to progression of thoracolumbar kyphosis in children with achondroplasia: a retrospective cohort study of forty-eight children treated in a comprehensive orthopaedic center. Spine 34, 1699–1705 (2009).
65. Kopits, S. E. Thoracolumbar kyphosis and lumbosacral hyperlordosis in achondroplastic children. Basic Life Sci. 48, 241–255 (1988).
66. Margalit, A., Mckean, G., Lawing, C., Galey, S. & Ain, M. C. Walking out of the curve: thoracolumbar kyphosis in achondroplasia. J. Pediatr. Orthop. 38, 491–497 (2018).
67. Rosenfeld, R. M. et al. Clinical practice guideline: otitis media with effusion executive summary (Update). Otolaryngol. Head Neck Surg. 154, 201–214 (2016).
68. Afsharpaiman, S., Sillence, D., Sheikhvatan, M., Ault, J. & Waters, K. Respiratory events and obstructive sleep apnea in children with achondroplasia: investigation and treatment outcomes. Sleep Breath. 15, 755–761(2011).
69. Julliand, S. et al. Lung function, diagnosis, and treatment of sleep-disordered breathing in children with achondroplasia. Am. J. Med. Genet. A 158A, 1987–1993 (2012).
70. Tenconi, R. et al. Sleep-disordered breathing and its management in children with achondroplasia. Am. J. Med. Genet. A 173, 868–878 (2017).
71. Inan, M., Jeong, C., Chan, G., Mackenzie, W. G. & Glutting, J. Analysis of lower extremity alignment in achondroplasia. J. Pediatr. Orthop. 26, 75–78 (2006).
72. Vaidya, S. V. et al. Bifocal tibial corrective osteotomy with lengthening in achondroplasia: an analysis of results and complications. J. Pediatr. Orthop. 26, 788–793 (2006).
73. Al-Saleem, A. & Al-Jobair, A. Achondroplasia: craniofacial manifestations and considerations in dental management. Saudi Dent. J. 22, 195–199 (2010).
74. Hecht, J. T. et al. Obesity in achondroplasia. Am. J. Med. Genet. 31, 597–602 (1988).
75. White, K. K. et al. Best practice guidelines for management of spinal disorders in skeletal dysplasia. Orphanet J. Rare Dis. 15, 161 (2020).
76. Takken, T., Van Bergen, M. W. M., Sakkers, R. J. B., Helders, P. J. M. & Engelbert, R. H. H. Cardiopulmonary exercise capacity, muscle strength, and physical activity in children and adolescents with achondroplasia. J. Pediatr. 150, 26–30 (2007).
77. Van Brussel, M., Van Der Net, J., Hulzebos, E., Helders, P. J. M. & Takken, T. The Utrecht approach to exercise in chronic childhood conditions: the decade in review. Pediatr. Phys. Ther. 23, 2–14 (2011).
78. Okenfuss, E., Moghaddam, B. & Avins, A. L. Natural history of achondroplasia: a retrospective review of longitudinal clinical data. Am. J. Med. Genet. A 182, 2540–2551 (2020).
79. Bodensteiner, J. B. Neurological manifestations of achondroplasia. Curr. Neurol. Neurosci. Rep. 19, 105 (2019).
80. Carlisle, E. S. et al. Laminectomy in patients with achondroplasia. Spine 36, 886–892 (2011).
81. Fredwall, S. O. et al. Obstructive sleep apnea in Norwegian adults with achondroplasia: a population-based study. Orphanet J. Rare Dis. 16, 156 (2021).
82. Glass, L., Shapiro, I., Hodge, S. E., Bergstrom, L. & Rimoin, D. L. Audiological findings of patients with achondroplasia. Int. J. Pediatr. Otorhinolaryngol. 3, 129–135 (1981).
83. Tunkel, D. et al. Hearing loss in skeletal dysplasia patients. Am. J. Med. Genet. A 158A, 1551–1555 (2012).
84. Hoover-Fong, J. et al. Blood pressure in adults with short stature skeletal dysplasias. Am. J. Med. Genet. A 182, 150–161 (2020).
85. Madsen, A., Fredwall, S. O., Maanum, G., Henriksen, C. & Slettahjell, H. B. Anthropometrics, diet, and resting energy expenditure in Norwegian adults with achondroplasia. Am. J. Med. Genet. A 179, 1745–1755 (2019).
86. Sciubba, D. M. et al. Spinal stenosis surgery in pediatric patients with achondroplasia. J. Neurosurg. 106, 372–378 (2007).
87. Fredwall, S. O. et al. Cardiovascular risk factors and body composition in adults with achondroplasia. Genet. Med. 23, 732–739 (2021).
88. Hunter, A. G., Bankier, A., Rogers, J. G., Sillence, D. & Scott, C. I. Medical complications of achondroplasia: a multicentre patient review. J. Med. Genet. 35, 705–712 (1998).
89. Hall, J. G. Kyphosis in achondroplasia: probably preventable. J. Pediatr. 112, 166–167 (1988).
90. Siebens, A. A., Hungerford, D. S. & Kirby, N. A. Achondroplasia: effectiveness of an orthosis in reducing deformity of the spine. Arch. Phys. Med. Rehabil. 68, 384–388 (1987).
91. Pyeritz, R. E., Sack, G. H., Udvarhelyi, G. B., Opitz, J. M. & Reynolds, J. F. Thoracolumbosacral laminectomy in achondroplasia: long-term results in 22 patients. Am. J. Med. Genet. 28, 433–444 (1987).
92. Jeong, S.-T. et al. MRI study of the lumbar spine in achondroplasia. a morphometric analysis for the evaluation of stenosis of the canal. J. Bone Joint Surg. Br. 88, 1192–1196 (2006).
93. Brooks, J. T., Bernholt, D. L., Tran, K. V. & Ain, M. C. The tibial slope in patients with achondroplasia: its characterization and possible role in genu recurvatum development. J. Pediatr. Orthop. 36, 349–354 (2016).
94. Kopits, S. E. Orthopedic aspects of achondroplasia in children. Basic Life Sci. 48, 189–197 (1988).
95. Bailey, J. A. Orthopaedic aspects of achondroplasia. J. Bone Joint Surg. Am. 52, 1285–1301 (1970).
96. Okura, T. et al. Activated FGFR3 prevents subchondral bone sclerosis during the development of osteoarthritis in transgenic mice with achondroplasia. J. Orthop. Res. 36, 300–308 (2018).
97. Sabharwal, S. & Zhao, C. Assessment of lower limb alignment: supine fluoroscopy compared with a standing full-length radiograph. J. Bone Joint Surg. Am. 90, 43–51 (2008).
98. Sabharwal, S. et al. Reliability analysis for radiographic measurement of limb length discrepancy. J. Pediatr. Orthop. 27, 46–50 (2007).
99. Whitaker, A. & Vuillermin, C. Lower extremity growth and deformity. Curr. Rev. Musculoskelet. Med. 9, 454–461 (2016).
100. Mcclure, P. K., Kilinc, E. & Birch, J. G. Growth modulation in achondroplasia. J. Pediatr. Orthop. 37, e384–e387 (2017).
101. Akyol, Y. et al. Magnetic resonance evaluation of the knee in children and adolescents with achondroplasia. Pediatr. Radiol. 45, 888–895 (2015).
102. Atanda, A., Wallace, M., Bober, M. B. & Mackenzie, W. Arthroscopic treatment of discoid lateral meniscus tears in children with achondroplasia. J. Pediatr. Orthop. 36, e55–e58 (2016).
103. Hoernschemeyer, D. G., Atanda, A., Dean-Davis, E. & Gupta, S. K. Discoid meniscus associated with achondroplasia. Orthopedics 39, e498–e503 (2016).
104. Leiva-Gea, A. et al. Staged upper and lower limb lengthening performing bilateral simultaneous surgery of the femur and tibia in achondroplastic patients. Arch. Orthop. Trauma Surg. 140, 1665–1676 (2020).
105. Launay, F. et al. Fracture following lower limb lengthening in children: a series of 58 patients. Orthop. Traumatol. Surg. Res. 99, 72–79 (2013).
106. Matsushita, M. et al. Physical, mental, and social problems of adolescent and adult patients with achondroplasia. Calcif. Tissue Int. 104, 364–372 (2019).
107. Balci, H. I. et al. Bilateral humeral lengthening in achondroplasia with unilateral external fixators. Bone Joint J. 97-B, 1577–1581 (2015).
108. Ginebreda, I. et al. Surgical technique and outcomes for bilateral humeral lengthening for achondroplasia: 26-year experience. Musculoskelet. Surg. 103, 257–262 (2019).
109. Shadi, M., Musielak, B., Koczewski, P. & Janusz, P. Humeral lengthening in patients with achondroplasia and in patients with post-septic shortening: comparison of procedure efficiency and safety. Int. Orthop. 42, 419–426 (2018).
110. Bloemeke, J. et al. Cross-cultural selection and validation of instruments to assess patient-reported outcomes in children and adolescents with achondroplasia. Qual. Life Res. 28, 2553–2563 (2019).
111. Collins, W. O. & Choi, S. S. Otolaryngologic manifestations of achondroplasia. Arch. Otolaryngol. Head Neck Surg. 133, 237–244 (2007).
112. Lyford-Pike, S., Hoover-Fong, J. & Tunkel, D. E. Otolaryngologic manifestations of skeletal dysplasias in children. Otolaryngol. Clin. North Am. 45, 579–598 (2012).
113. Sisk, E. A., Heatley, D. G., Borowski, B. J., Leverson, G. E. & Pauli, R. M. Obstructive sleep apnea in children with achondroplasia: surgical and anesthetic considerations. Otolaryngol. Head Neck Surg. 120, 248–254 (1999).
114. Afsharpaiman, S., Saburi, A. & Waters, K. A. Respiratory difficulties and breathing disorders in achondroplasia. Paediatr. Respir. Rev. 14, 250–255 (2013).
115. Zaffanello, M. et al. Sleep disordered breathing in children with achondroplasia. World J. Pediatr. 13, 8–14 (2017).
116. Ednick, M. et al. Sleep-related respiratory abnormalities and arousal pattern in achondroplasia during early infancy. J. Pediatr. 155, 510–515.e511 (2009).
117. Dessoffy, K. E., Modaff, P. & Pauli, R. M. Airway malacia in children with achondroplasia. Am. J. Med. Genet. A 164A, 407–414 (2014).
118. Susarla, S. M. et al. Subcranial and orthognathic surgery for obstructive sleep apnea in achondroplasia. J. Craniomaxillofac. Surg. 45, 2028–2034 (2017).
119. Rosenfeld, R. M. et al. Clinical practice guideline: tympanostomy tubes in children — executive summary. Otolaryngol. Head Neck Surg. 149, 8–16 (2013).
120. Pauli, R. M. & Modaff, P. Jugular bulb dehiscence in achondroplasia. Int. J. Pediatr. Otorhinolaryngol. 48, 169–174 (1999).
121. Stephen, L., Holmes, H., Roberts, T., Fieggen, K. & Beighton, P. Orthodontic management of achondroplasia in South Africa. S. Afr. Med. J. 95, 588–589 (2005).
122. Machado-Júnior, A., Zancanella, E. & Crespo, A. Rapid maxillary expansion and obstructive sleep apnea: a review and meta-analysis. Med. Oral. Patol. Oral. Cir. Bucal 21, e465–e469 (2016).
123. Mayhew, J. F., Katz, J., Miner, M., Leiman, B. & Hall, I. D. Anaesthesia for the achondroplastic Dwarf. Can. Anaesth. Soc. J. 33, 216–221 (1986).
124. Zucconi, M. et al. Sleep and upper airway obstruction in children with achondroplasia. J. Pediatr. 129, 743–749 (1996).
125. Merker, A. et al. Growth in achondroplasia: development of height, weight, head circumference, and body mass index in a European cohort. Am. J. Med. Genet. A 176, 1723–1734 (2018).
126. Schulze, K. J., Alade, Y. A., McGready, J. & Hoover-Fong, J. E. Body mass index (BMI): the case for condition-specific cut-offs for overweight and obesity in skeletal dysplasias. Am. J. Med. Genet. A 161, 2110–2112 (2013).
127. Rohenkohl, A. C., Bullinger, M. & Quitmann, J. Quality of life in children, adolescents, and young adults with achondroplasia. Orthopade 44, 212–218 (2015).
128. Sommer, R. et al. An Icf-Cy-based approach to assessing self- and observer-reported functioning in young persons with achondroplasia – development of the pilot version of the Achondroplasia Personal Life Experience Scale (APLES). Disabil. Rehabil. 39, 2499–2503 (2017).
129. Cortinovis, I., Luraschi, E., Intini, S., Sessa, M. & Delle Fave, A. The daily experience of people with achondroplasia. Appl. Psychol. Health Well-Being 3, 207–227 (2011).
130. Witt, S. et al. Quality of life of children with achondroplasia and their parents – a German cross-sectional study. Orphanet J. Rare Dis. 14, 194 (2019).
131. Thompson, S., Shakespeare, T. & Wright, M. J. Medical and social aspects of the life course for adults with a skeletal dysplasia: a review of current knowledge. Disabil. Rehabil. 30, 1–12 (2008).
132. Gómez-Zúñiga, B., Pulido Moyano, R., Pousada Fernández, M., García Oliva, A. & Armayones Ruiz, M. The experience of parents of children with rare diseases when communicating with healthcare professionals: towards an integrative theory of trust. Orphanet J. Rare Dis. 14, 159 (2019).
133. Witt, S. et al. Understanding, assessing and improving health-related quality of life of young people with achondroplasia – a collaboration between a patient organization and academic medicine. Pediatr. Endocrinol. Rev. 15, 109–118 (2017).
134. Savarirayan, R. et al. C-type natriuretic peptide analogue therapy in children with achondroplasia. N. Engl. J. Med. 381, 25–35 (2019).
135. Savarirayan, R. et al. Once-daily, subcutaneous vosoritide therapy in children with achondroplasia: a randomised, double-blind, phase 3, placebo-controlled, multicentre trial. Lancet 396, 684–692 (2020).